Reynolds-Finley Section
Die aetiologie, der bergriff und die prophylaxis des kindbettfiebers. Pest, Wien und Leipzig: C. A. Hartleben, 1861.
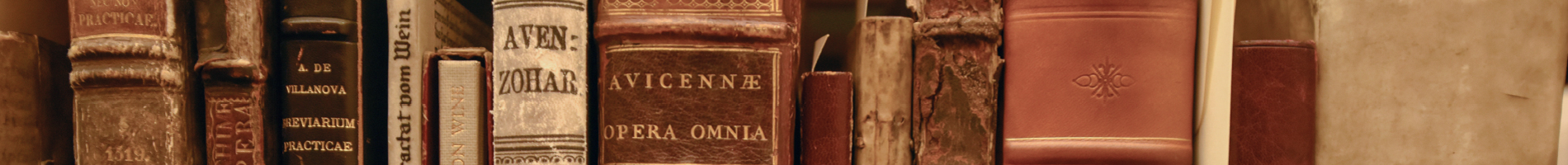
 Ignaz Semmelweis, a Hungarian obstetrician working in Vienna in the mid-nineteenth century, made a crucial discovery about puerperal fever that helped usher in the use of antiseptics. In 1846, the Vienna General Hospital (Allgemeines Krankenhaus) had two obstetrics clinics, and Semmelweis was a surgeon, clinician, and instructor of medical students in the first clinic. The second clinic was only different in that it was used for the instruction of midwives instead of physicians. It was, therefore, baffling that the second had such a drastically smaller percentage of patient deaths by puerperal fever (childbed fever), an infection that occurs after childbirth or abortion. The first clinic had attained such a reputation for deaths by the fever that women cried and begged not to be taken into it (Garrison 435). Semmelweis, in an attempt to resolve this problem in his clinic, began studying autopsies of puerperal fever fatalities. When his friend and former instructor, Kolletschka, died of an infected wound accidentally inflicted during a postmortem dissection, Semmelweis was present during this autopsy also. Because of his careful observations of puerperal fever victims, he was able to recognize that these women had experienced the same pathological changes as Kolletschka did from his infected wound. He deduced that puerperal fever, like Kolletschka’s disease was transmitted through the blood, and that medical students were bringing it into the first clinic from the dissection table. Semmelweis noticed that the medical students in the first clinic, unlike the midwives in the second, were treating women directly after dissections and without washing their hands. Once he instated a policy requiring the students to wash their hands and scrub them in chlorine water before examining women, the clinic’s puerperal fever death rate drastically dropped (Clendening 603-604). When he extended the policy to cover all instruments used on laboring women, he practically eliminated the fever from his hospital (Dict. Sci. Bio., Vol. 11&12, p. 295).
Ignaz Semmelweis, a Hungarian obstetrician working in Vienna in the mid-nineteenth century, made a crucial discovery about puerperal fever that helped usher in the use of antiseptics. In 1846, the Vienna General Hospital (Allgemeines Krankenhaus) had two obstetrics clinics, and Semmelweis was a surgeon, clinician, and instructor of medical students in the first clinic. The second clinic was only different in that it was used for the instruction of midwives instead of physicians. It was, therefore, baffling that the second had such a drastically smaller percentage of patient deaths by puerperal fever (childbed fever), an infection that occurs after childbirth or abortion. The first clinic had attained such a reputation for deaths by the fever that women cried and begged not to be taken into it (Garrison 435). Semmelweis, in an attempt to resolve this problem in his clinic, began studying autopsies of puerperal fever fatalities. When his friend and former instructor, Kolletschka, died of an infected wound accidentally inflicted during a postmortem dissection, Semmelweis was present during this autopsy also. Because of his careful observations of puerperal fever victims, he was able to recognize that these women had experienced the same pathological changes as Kolletschka did from his infected wound. He deduced that puerperal fever, like Kolletschka’s disease was transmitted through the blood, and that medical students were bringing it into the first clinic from the dissection table. Semmelweis noticed that the medical students in the first clinic, unlike the midwives in the second, were treating women directly after dissections and without washing their hands. Once he instated a policy requiring the students to wash their hands and scrub them in chlorine water before examining women, the clinic’s puerperal fever death rate drastically dropped (Clendening 603-604). When he extended the policy to cover all instruments used on laboring women, he practically eliminated the fever from his hospital (Dict. Sci. Bio., Vol. 11&12, p. 295).
Despite opposition from professional peers, Semmelweis stood by his findings and pioneered the use of antiseptics in obstetrics. By working hard to improve conditions for obstetrics wards in both Hungary and Vienna, he holds a place in the history and advancement of obstetrics as well as for discovering that puerperal fever is caused by microorganisms transmitted through the blood stream (Garrison & Morton 6277). The Reynolds-Finley Library has a first edition copy of his book, Die aetiologie, der bergriff und die prophylaxis des kindbettfiebers, or “The cause, concept and prevention of child-bed fever”, which was published in 1861. The work was not well received by the prominent physicians of the day, and it prompted conflicts which took their toll on Semmelweis. He was eventually committed to an insane asylum and died a few weeks later, ironically of an infection caused by a wound.
Clendening, Source Book of Med. Hist., pp. 603-604; Dict. Sci. Bio., Vol. 11&12, pp. 294-296; Garrison, Hist. of Med., 4th Edition, pp. 435; Garrison & Morton, Med. Bib., 5th Edition, 6277; Reynolds Historical Library, Rare books and coll…, 3748.
Image: Ignaz Semmelweis, Print Collection, Reynolds-Finley Historical Library.
An account of the bilious remitting yellow fever, as it appeared in the city of Philadelphia, in the year 1793. Philadelphia: printed by Thomas Dobson, 1794.
Medical inquiries and observations, upon the diseases of the mind. Philadelphia: Kimber & Richardson, 1812.
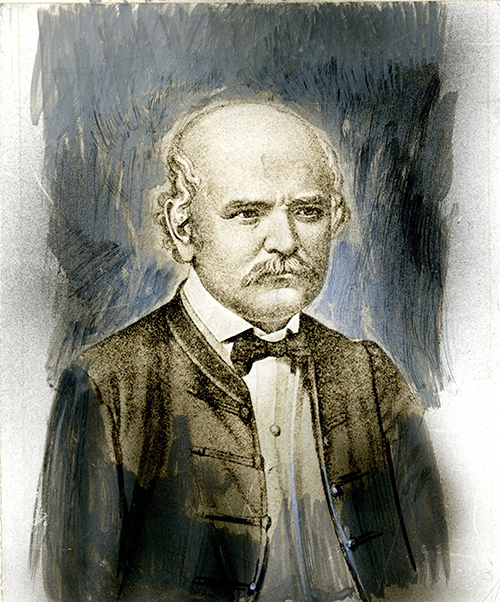
 A native of Pennsylvania, Benjamin Rush went to medical school in Edinburgh, recognizing the value of a European medical education in the success of American physicians of his day (Duffy 63). He taught chemistry and medicine at the College of Philadelphia and the University of Pennsylvania, was a physician at the Pennsylvania Hospital, and later in life, became the Treasurer of the United States Mint. Also, Rush took an active interest in public policy and humanitarian reform issues, such as slavery, alcoholism, and the death penalty. He was in the Second Continental Congress and signed the Declaration of Independence. He founded the Philadelphia Dispensary and promoted the public school system and female education. Medical historian John Duffy explains that “The combination of his political, philanthropic, and medical activities soon gained Rush a reputation as America’s outstanding physician” (64).
A native of Pennsylvania, Benjamin Rush went to medical school in Edinburgh, recognizing the value of a European medical education in the success of American physicians of his day (Duffy 63). He taught chemistry and medicine at the College of Philadelphia and the University of Pennsylvania, was a physician at the Pennsylvania Hospital, and later in life, became the Treasurer of the United States Mint. Also, Rush took an active interest in public policy and humanitarian reform issues, such as slavery, alcoholism, and the death penalty. He was in the Second Continental Congress and signed the Declaration of Independence. He founded the Philadelphia Dispensary and promoted the public school system and female education. Medical historian John Duffy explains that “The combination of his political, philanthropic, and medical activities soon gained Rush a reputation as America’s outstanding physician” (64).
When the yellow fever epidemic of Philadelphia broke out in 1793, Rush was already known for his clinical observations of diseases such as cholera, dengue, and thermal fever. Instead of fleeing the city like many other doctors, Rush remained, treating as many as 100-150 patients daily. His observations about the fever’s course, causes, and treatment are noted in his epidemiology classic, An account of the bilious remitting yellow fever, of which the Reynolds-Finley Library has a first edition copy. Here, he advocates a treatment of abundant bloodletting, cooling of the body, and doses of calomel (a form of mercury) and jalap (Garrison 379-380). To the dismay of many in the community, Rush also proposes that the epidemic was brought on by city sanitation problems instead of being imported (Not. Med. Books 147). Despite professional opposition to his treatments and ideas of causation, Rush’s theories prevailed, and because of his own popularity, were adopted for years to come, especially in the American West and South. The negative result was that these heroic therapies (i.e., excessive purging, bloodletting and mercury) made their way into American medical practice (Duffy 65). On the other hand, Rush’s ideas sparked the movement towards public health and hygiene in the 1800s (Duffy 68).
The Reynolds-Finley Library also has a first edition copy of Benjamin Rush’s Medical inquiries and observations, upon the diseases of the mind, the first American psychiatric writing. Knowledge for this work was acquired while he was in charge of the insane at Pennsylvania Hospital and by his unorthodox teaching of psychiatry in his physiology lectures. Rush recognized that behavior and emotions can be disturbed just like the intellect, a great contribution to the field of psychiatry (Dict. Sci. Bio., Vol. 11-12, 617).
There is also a handwritten letter by Dr. Rush, dated January 13, 1797, located in the UAB Archives.
Cambridge Illus. Hist. Med., p. 124; Dict. Sci. Bio., Vol. 11-12, pp. 616-617; Duffy, From Humors to Med. Sci.…pp. 63-68; Garrison, Hist. of Med., 4th Edition, pp. 379-380; Oxford Comp. to Med., Vol. II, p. 1284; Not. Med. Books,p. 147; Reynolds Historical Library, Rare books and coll…, 3643 & 3649.
Image: Benjamin Rush, Print Collection, Reynolds-Finley Historical Library.
“Eine neue art von strahlen.” [In: Sitzungsberichten der Würzburger Physik-medic. Gesellschaft. 1895] Würzburg, Stahel, 1895.
“Eine neue art von strahlen. II. Mittheilung.” [In: Sitzungsberichten der Würzburger Physikal-medic. Gesellschaft…]. Würzburg, Stahel, 1896.
“On a new kind of rays.” [In] Nature, v. 53, no. 1369, January 23, 1896. London, 1896.
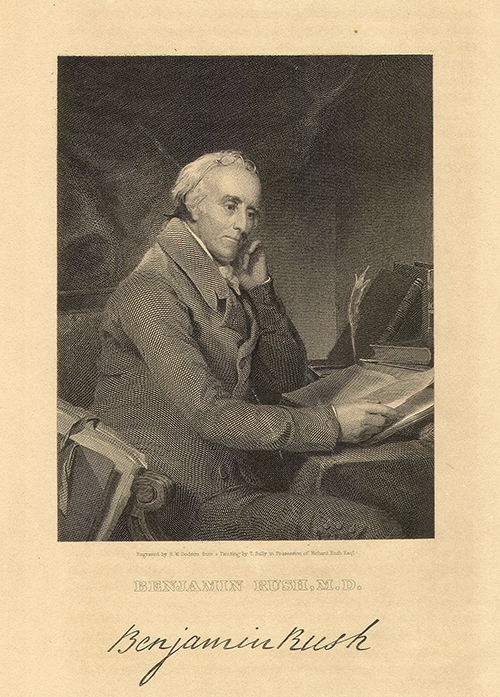
 Near the end of the 19th century, there was an innovation which proved to be instantly useful in medical diagnosis, and eventually showed its value in treatment and therapy too. This new device was called the x-ray by its discoverer, Wilhelm Conrad Röntgen, but other scientists called it the Röntgen ray out of respect. Though born in Lennep in the Rhine Province of Germany, Röntgen spent most of his childhood in Holland. As a student, he did not excel, and his opportunities were further limited by his expulsion from one school for not snitching on a classmate. However, this all changed when he began studying mechanical engineering at the Polytechnic in Zurich, and even more so when he became an assistant to the professor of physics, August Kundt. Thanks to the help of this mentor, and to Röntgen’s own hard work in publishing, he held several respected academic positions before his ground-breaking discovery (Dict. Sci. Bio., Vol. 11 & 12, p. 529).
Near the end of the 19th century, there was an innovation which proved to be instantly useful in medical diagnosis, and eventually showed its value in treatment and therapy too. This new device was called the x-ray by its discoverer, Wilhelm Conrad Röntgen, but other scientists called it the Röntgen ray out of respect. Though born in Lennep in the Rhine Province of Germany, Röntgen spent most of his childhood in Holland. As a student, he did not excel, and his opportunities were further limited by his expulsion from one school for not snitching on a classmate. However, this all changed when he began studying mechanical engineering at the Polytechnic in Zurich, and even more so when he became an assistant to the professor of physics, August Kundt. Thanks to the help of this mentor, and to Röntgen’s own hard work in publishing, he held several respected academic positions before his ground-breaking discovery (Dict. Sci. Bio., Vol. 11 & 12, p. 529).
While rector and director of the Institute of Physics at the University of Würzburg, Röntgen experimented with the Crookes tube, a vacuum that interested him because of its usefulness in the study of electricity. He noticed by accident that the tube produced shadows of objects on a photographic plate. But it was through carefully planned experimentation that he showed how the same process done to a light-proof tube results in a kind of ray that passes through the soft parts of the body, revealing internal bones and organs (Clendening 666; Garrison 721). Quickly, Röntgen revealed his discovery to the Würzburg Society by presenting a paper entitled “Eine neue art von strahlen,” which translates into English as “On a new kind of rays.” Attending the presentation was the respected histologist, Rudolph Albert von Kölliker, who volunteered to have an x-ray of his hand made. The demonstration impressed all attendees, and Kölliker’s suggestion of the term Röntgen ray was well received. The society published the paper in its journal for December 1895. The Reynolds-Finley has a boxed set including two copies of the first publication of the paper, and one copy of a follow-up paper published in the same journal. Potential medical uses of the x-ray were instantly recognized. Some of the earliest benefits concerned orthopedics and diagnosis of chest difficulties (Cambridge 140-1). News spread throughout the world, and the paper was quickly translated into many languages. The Reynolds-Finley has a copy of the 1896 English translation from the journal Nature. Röntgen’s great discovery earned him the Nobel Prize for Physics in 1901, and many scholars hold this technology as the most influential to medicine (Duffin 202).
Cambridge Illus. Hist. Med., pp. 140-141; Clendening, Source Book of Med. Hist., p. 666; Dict. Sci. Bio., Vol. 11 & 12, p. 529; Duffin, Hist. of Med., p. 202; Garrison, Hist. of Med. 4th Edition, p. 721; One Hund. Books, 83; Reynolds Historical Library, Rare books and coll., 3584, 3585 & 3590.
Image: Wilhelm Conrad Rontgen, Print Collection, Reynolds-Finley Historical Library.
Ninth Book of the Al’Mansuri. With commentary of Geraldus de Solo. Translated into Hebrew by Tobiel ben Samuel de Leiria. Portugal, 1388.
 During the Middle Ages, the Arab world preserved the knowledge of the Greeks and Romans and continued to flourish intellectually while Europe lay dormant. One of the great Arab physicians of that era was Al-Razi, known in the West as Rhazes. Born in Persia, he studied in Baghdad, Palestine, Egypt and Spain. Later he taught and directed hospitals in his home town, Rayy, Persia, and in Baghdad, where he became court physician. Rhazes also studied and wrote philosophical works, but these were not as well received as his medical writings. It was his descriptive and original clinical histories in the Hippocratic tradition that have gained him respect throughout history.
During the Middle Ages, the Arab world preserved the knowledge of the Greeks and Romans and continued to flourish intellectually while Europe lay dormant. One of the great Arab physicians of that era was Al-Razi, known in the West as Rhazes. Born in Persia, he studied in Baghdad, Palestine, Egypt and Spain. Later he taught and directed hospitals in his home town, Rayy, Persia, and in Baghdad, where he became court physician. Rhazes also studied and wrote philosophical works, but these were not as well received as his medical writings. It was his descriptive and original clinical histories in the Hippocratic tradition that have gained him respect throughout history.
Rhazes is well-known for his description of smallpox and measles, the first authentic account of these diseases (Garrison 129). He was also the first to distinguish these two diseases from each other and to propose the theory of acquired immunity by recognizing that individuals surviving smallpox never get it again (Garrison & Morton, 5441 & 2527.99). Other contributions to the field of medicine include several innovations in pharmacy and chemistry. He developed many chemical apparatuses used up to the beginning of the twentieth century, and he wrote a manual that classified chemicals and described procedures for their mixing and preparation that were later adopted by the Western world (Flannery 6).
Based primarily on Greek medicine, the Al’ Mansuri is Rhazes’s ten part textbook and encyclopedia of medicine. The title of the Ninth Book translates into English as Exposition of the ninth part of Rhazes (dealing with) the diseases from head to foot (Flannery 6). This famous pathology textwas used in the teaching of therapeutics until well after the Renaissance (Garrison 129). Since the ninth book was so popular, it was often published alone (Sarton 609). One of the Reynolds-Finley Historical Library’s oldest and most rare materials is a Hebrew translation of the Ninth Book of Al’Mansuri which was completed in 1388. The translator is Tobiel ben Samuel, who identifies himself in the introduction as a Jewish physician from Portugal and student of Moses de Leira. Tobiel translated the work from the Latin version done by famous professor, Gerard de Solo of Montpellier University, in 1344. Of the three known translations of this text, the Reynolds-Finley copy is the only one with the original title page, preface and other introductory material intact (Flannery 5). And it is important culturally as a symbol of the Arabic preservation and advancement of knowledge in the Middle Ages and the role of Jewish scholarship in transferring it to the West (Flannery 6).
Flannery, [In] The Watermark, Vol. 23, No. 1, Winter, 1999-2000, pp. 5-7; Garrison, Hist. Med.,4th Edition, p. 129; Garrison & Morton, Med. Bib., 5th Edition, 2527.99 & 5441; Heirs of Hippocrates, 34-36; Reynolds Historical Library, Rare books and coll…, 5088; Sarton, Intro. to the Hist. of Sci., Vol. I, p. 609.
Image: Portrait of Rhazes (al-Razi) (AD 865 - 925) physician and alchemist who lived in Baghdad. Wellcome Images Wellcome Library, London.